ABMI
Main menu:
- Home
- About ABMI
- Clinical Focus
- Monitoring Software
- TCD Systems
- Clinical Studies
- News/Investors
- Contact Us
Monitoring Brain Embolization
Clinical Focus
Monitoring Brain Embolization in the Operating Room
As it is more and more obvious that peri-operative embolization causes stroke, TIA and neuropsychological losses, resulting in death, handicap and cognitive decline, surgeons and interventionists are increasingly interested by monitoring solutions for asserting the risk of stroke and acting immediately through neuroprotective therapy.
Indeed, there is no "traditional" way of assessing the neurological condition of a patient when he/she is under total anesthesia! A traditional clinical exam can be performed only after the patient has sufficiently woken up, and by then it is too late to act with stroke-treating or neuroprotective drugs (which have to be administered within 3-6 hours after stroke onset).
The new paradigm in peri-operative stroke protection we at ABMI are introducing, is that of peri-operative real-time monitoring of blood flows and brain embolization.
Thereby, upon measuring a brain embolization load over some clinically defined threshold, the patient would be given the necessary medication right upon stroke onset, or the surgical procedure would be changed or altered in such a way as to reduce embolization!
Let us note that in such a peri-operative neuromonitoring scheme, differentiating the solid and gaseous emboli - as ABMI expert systems do - is essential since neuroprotective therapy should be introduced only in the case of solid emboli.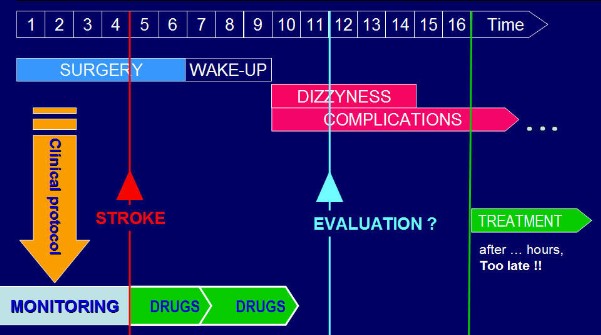
Monitoring Embolization during Percutaneous Stenting
The number of percutaneous transluminal procedures has been increasing rapidly over the last years, as the graph below clearly shows. Percutaneous artery stenting is actually replacing traditional "open-sky" surgery in pathologies such as coronary stenoses, carotid stenoses, and intracranial stenoses and aneurisms, among others.
Even more than classic surgery, percutaneous stenting carries a risk of brain embolization. This is critical to the point that specific protection devices have been developed, such as intra-arterial filters. These filters however are unable to stop all emboli, and moreover the introduction of the filter is an additional procedure in itself which is prone to causing embolization.
As we do for the classic surgical OR, we at ABMI aim at putting on the market and making real-time monitoring of embolization a standard procedure during stenting - a procedure that would allow to assert brain embolization both in the angiography suite and in the recovery room.
And here too the solid/gas differentiation is essential! Indeed, during angiography-monitored stenting the interventional radiologist uses contrast agent to visualize the artery, and such contrast agent is made of tiny air bubbles which are heard on a transcranial Doppler as emboli. Differentiating these form threatening solid emboli due to plaque disruption - e.g. during stenosis pre-dilation or stent dilation - is key to an effective neuroprotection therapy.
Sub-Menu:
- Some Facts about Stroke
- Transcranial Doppler (TCD)
- Monitoring Brain Embolization ←
- Neuroprotection during Carotid and Cardiac Surgery
- Typical Applications of ABMI Technology